Global warming, an inexorable phenomenon generated predominantly by anthropogenic activities, exerts far-reaching repercussions across multifaceted dimensions of society, including the realms of modern medicine and healthcare. As the planet’s temperature escalates, the ramifications on health and well-being intensify, presenting an intricate labyrinth that healthcare systems must navigate. This analysis will delve into the myriad ways in which global warming is reshaping the landscape of medical practice, public health policies, and the very fabric of healthcare delivery.
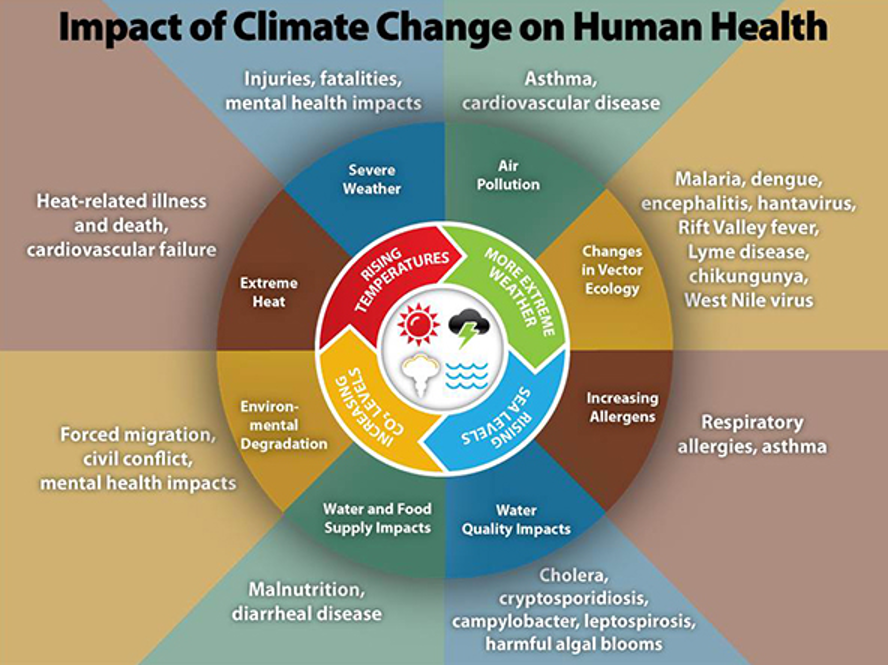
The immediate observation often encountered in discussions surrounding climate change is its impact on the prevalence of infectious diseases. Rising temperatures and fluctuating precipitation patterns create optimal conditions for vectors such as mosquitoes and ticks, fostering an environment conducive to the proliferation of diseases such as malaria, dengue fever, and Lyme disease. Historical data indicate a correlation between climatic shifts and the emergence of these infections in previously unaffected regions. For instance, the incursion of the Aedes aegypti mosquito into temperate regions has led to an uptick in dengue cases, reinforcing the notion that our changing climate is entwined with the dynamics of disease transmission.
Moreover, the alteration of ecosystems due to global warming does not merely facilitate vector habitat expansion; it also impacts the resilience of entire populations. Affected communities, particularly those in developing nations with limited healthcare infrastructure, face heightened vulnerability. The lens through which we observe these shifts unveils a stark reality: as the burden of endemic and emergent diseases burgeons, the healthcare system grapples under the strain of increased patient loads, necessitating a reevaluation of public health strategies.
Further compounding this issue is the interplay between climate-related environmental degradation and the exacerbation of chronic non-communicable diseases (NCDs). Air pollution, a direct byproduct of climate change, carries significant health implications. Pollutants such as particulate matter and ground-level ozone are notorious for exacerbating respiratory diseases, cardiovascular conditions, and even neurological disorders. The rise in heatwaves additionally imposes stress on cardiovascular systems, leading to increased mortality rates among vulnerable populations, including the elderly. Thus, the interdependence of global warming and chronic health conditions manifests as a dual challenge—one that encompasses both infectious diseases and the resurgence of chronic ailments.
Moreover, considering the psychosocial dimensions, the mental health toll attributed to climate change is profound. The anxiety and distress precipitated by natural disasters, food insecurity, and forced migrations contribute to a burgeoning mental health crisis. As communities face the specter of environmental upheaval, healthcare systems must afford attention not only to physical ailments but also to the psychological ramifications of such crises. The integration of mental health services into primary healthcare becomes imperative, underscoring the need for a holistic approach to health that acknowledges the complex relationship between environment and well-being.
Healthcare delivery systems themselves are not impervious to the effects of climate change. The infrastructure supporting modern medicine faces vulnerabilities as extreme weather events become more prevalent. Hospitals and healthcare facilities are often ill-prepared for the onslaught of such disturbances, leading to interrupted services during critical times. The cascading effects of environmental disasters necessitate contingency planning and resilient healthcare infrastructure capable of withstanding climate extremes, prompting policymakers and healthcare administrators to explore innovative solutions and adaptive strategies.
The ripple effects of global warming extend into pharmaceutical research and development as well. The disruption of global supply chains, spurred by climate-related events, jeopardizes the availability of essential medications and medical supplies. Ethical dilemmas arise in the pharmaceutical industry, where the pressures to rapidly deliver treatments may overshadow the need for sustainable production practices. As the health sector confronts these challenges, it is incumbent upon stakeholders to foster collaboration between environmental scientists and healthcare professionals, ensuring that developments in medical technology align with sustainability goals.
Education and training within the healthcare workforce must evolve alongside these challenges. As practitioners face an increasingly complex interplay of health determinants influenced by climate change, the need for interdisciplinary training becomes apparent. Future healthcare providers must be adept in not only diagnosing and treating diseases but also understanding the underlying environmental factors that contribute to health disparities. The integration of climate and health curricula into medical education is essential for cultivating a generation of healthcare professionals equipped to address the multifaceted challenges posed by global warming.
Collectively, the aforementioned factors coalesce to paint a vivid picture of the future landscape of healthcare in the shadow of global warming. A paradigm shift is necessary; healthcare systems must become agile entities that are not merely reactive to the health impacts of climate change but are proactive in mitigating these effects. This entails a commitment to sustainability, resilience, and equity in health—embracing practices that prioritize planetary health while simultaneously safeguarding human health outcomes.
In summation, the implications of global warming extend well beyond mere environmental concerns; they intricately weave into the very fabric of healthcare. From the resurgence of infectious diseases to the exacerbation of chronic illnesses, and from infrastructural vulnerabilities to the psychological toll on communities, the healthcare sector is at a crossroads. Addressing these challenges requires comprehensive strategies that resonate with the interconnectedness of health and environment, ultimately forging a path toward a more resilient and equitable healthcare system in the face of a warming world.






Leave a Comment